
In smokers, COPD develops 10–20 years earlier than in smokers with normal AAT levels. The leading manifestation of the disease in PiZZ individuals is chronic obstructive pulmonary disease (COPD) with early onset emphysema, particularly in smokers. This genetic defect results in the polymerisation of the AAT molecule in the hepatocytes, and the accumulation of the Z protein within the hepatocytes, leading to decreased release into the circulation. The main function of AAT is to inhibit neutrophil elastase and other serine proteases, including proteinase-3 and plasmin activator. The AAT deficiency is one of the most prevalent inherited disorders in populations of European descent, and it is characterised by low AAT levels in the serum and lungs. Severe alpha 1-antitrypsin (AAT) deficiency (PiZZ) is an autosomal, co-dominant, hereditary disorder. Early diagnosis of AAT deficiency is of utmost importance. The never-smoking PiZZ individuals identified by screening had a similar life expectancy to the never-smokers in the Swedish general population. By contrast, the risk of death was not increased in never-smoking PiZZ individuals identified by screening, compared to never-smoking controls, HR 1.2 (95% CI 0.6–2.2).
After adjustment for gender, age, smoking habits and presence of respiratory symptoms, the risk of death was still significantly higher for the PiZZ individuals than for the controls, hazard ratio (HR) 3.2 (95% CI 2.8–3.6 p<0.001). The PiZZ subjects had a significantly shorter survival time than the controls, p<0.001. During follow-up, 473 PiZZ subjects (30%), and 747 controls (12%) died. Median follow-up times for the PiZZ subjects (731 never-smokers) and controls (3179 never-smokers) were 12 and 17 years, respectively (p<0.001). Smoking habits were known for all subjects. The controls (n=5999) were randomly selected from the Swedish population register. The PiZZ subjects (n=1585) were selected from the Swedish National AATD Register. Our aim was to compare the survival of PiZZ individuals with randomly selected controls from the Swedish general population. The World Health Organization (WHO), American Thoracic Society (ATS), and the European Respiratory Society (ERS) recommend that everyone with COPD be tested for Alpha-1.Knowledge about the natural history of severe alpha 1-antitrypsin (AAT) deficiency (PiZZ) is limited.The most serious liver diseases are cirrhosis and liver cancer. Alpha-1 can also lead to liver disease.Up to 3% of all people diagnosed with COPD may have undetected Alpha-1.Alpha-1 is the most common known genetic risk factor for emphysema.Alpha-1 can lead to lung destruction and is often first diagnosed as asthma or smoking-related Chronic Obstructive Pulmonary Disease (COPD).Īlpha-1 cannot be diagnosed by symptoms or by a medical examination alone you need to get a simple, reliable blood test to know for sure.Carriers may pass the defective gene on to their children. People with one normal gene and one defective gene (for example MZ) are called “carriers”. An estimated 19 million people in the United States have one normal and one defective alpha-1 gene.Early diagnosis and avoiding risk factors, such as cigarette smoking, can help prevent Alpha-1 from causing disease. People with Alpha-1 may remain healthy throughout their lives.It is estimated that about 1 in every 2,500 Americans have Alpha-1. Alpha-1 has been identified in nearly all populations and ethnic groups.This leads to a build-up of abnormal AAT in the liver that can cause liver disease and a decrease of AAT in the blood that can lead to lung disease.

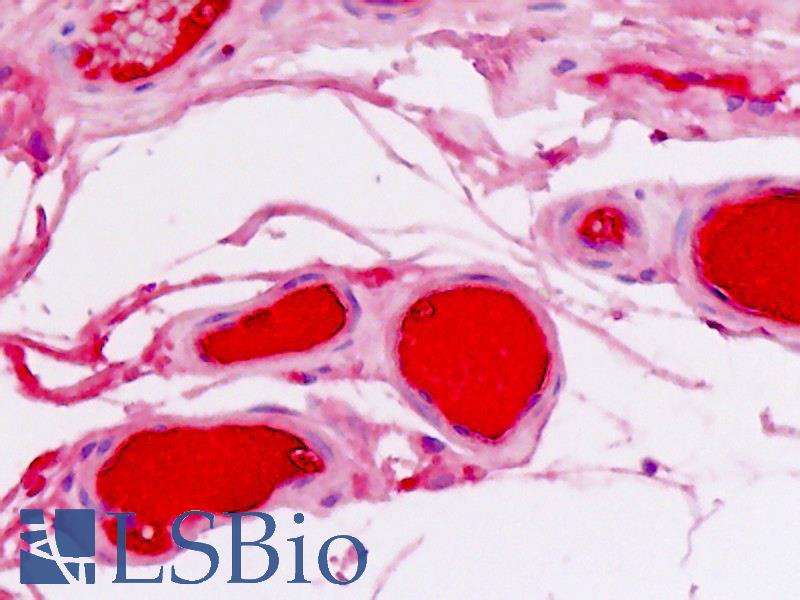
The low level of AAT in the blood occurs because the AAT is abnormal and cannot be released from the liver at the normal rate. The main function of AAT is to protect the lungs from inflammation caused by infection and inhaled irritants such as tobacco smoke. AAT, the alpha-1 protein, is mainly produced by the liver. Another deficient gene combination is SZ, although people with this gene combination are less likely to get lung or liver problems than those with two Z genes.Īlpha-1 occurs when there is a lack of a protein in the blood called alpha-1 antitrypsin, or AAT. Current evidence suggests that there are at least 100,000 people with Alpha-1 (ZZ) in the United States. People identified with Alpha-1 most commonly have two Z genes (ZZ). A person who does not have Alpha-1 will have two M genes (MM). The most common abnormal genes are called S and Z.

There are many types of abnormal alpha-1 antitrypsin genes.


 0 kommentar(er)
0 kommentar(er)
